Academician Zhong Nanshan and Professor Wang Deyun’s Team of SKLRD reveal aberrant epithelial cell proliferation in peripheral airways in bronchiectasis
2020-04-021928Recently, the original research paper titled "Aberrant epithelial Cell Proliferation in Peripheral Airways in Bronchiectasis” was published online in Frontiers in Cell and Developmental Biology by Academician Zhong Nanshan, Distinguished Professor Wang Deyun and Associate Researcher Guan Weijie as co-corresponding authors. The co-first authors of the paper are Dr. Peng Yang, Master Xu Airu, and Master Chen Shiying of Guangzhou Medical University.

The causes of bronchiectasis are diverse, and the pathogenesis has not been identified. Acute and chronic respiratory infections and recurrent bronchial obstruction can cause bronchial inflammation, destruction of the bronchial wall structure and secondary irreversible changes in bronchi and bronchiectasis. Reviewing the literature, it is found that the repair of airway damage is closely related to the proliferation and differentiation of epithelial progenitor cells; however, the correlation between the proliferation of progenitor cells and the occurrence and development of bronchiectasis in the peripheral airways in bronchiectasis is rarely reported. The process of airway epithelial cell repair is mainly completed by epithelial progenitor cells. The peripheral airway mainly includes the following three progenitor cells: basal cells (partly stem cells), Clara cells and type II alveolar epithelial cells. In this study, multiple immunofluorescence staining and immunohistochemical staining were used to explore multiple markers (TTF-1, P63, CC10, SPC, etc.) of epithelial progenitor cells in the peripheral airway, and a comprehensive evaluation was conducted based on the changes in inflammatory cells (neutrophils, Eosinophils, CD4+ T cells, CD8+ T cells, etc.) and clinical data of patients.
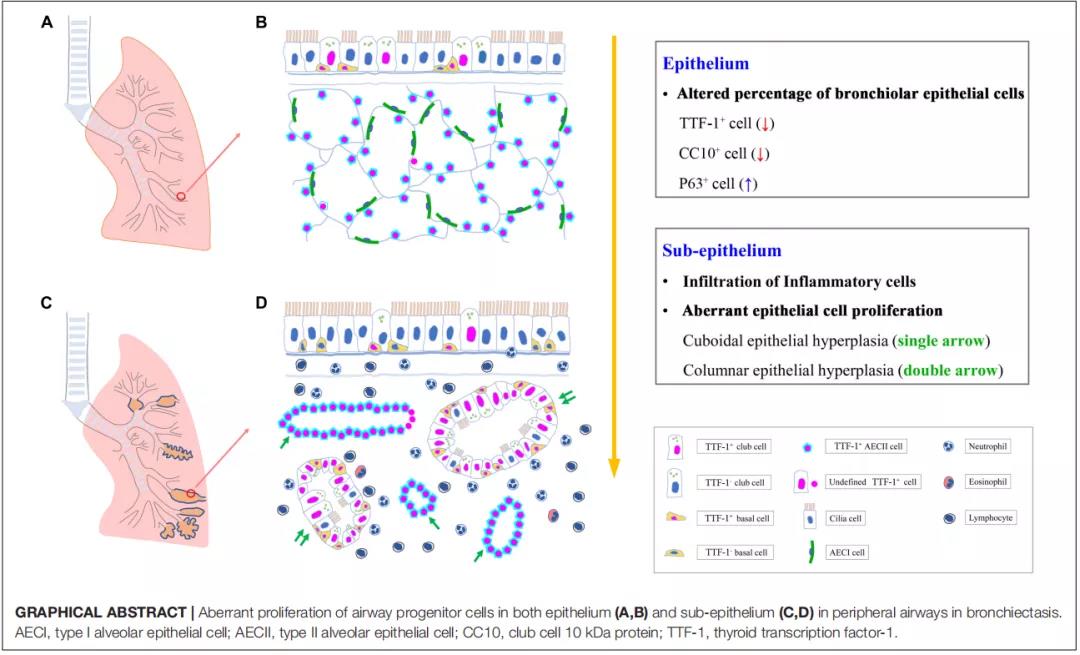
Aberrant proliferation of cells in peripheral airway epithelium (A, B) and subepithelial (C, D) groups in patients with bronchiectasis
The study found that both the dilated bronchiolar epithelium and subepithelial regions had aberrant progenitor cell proliferation. Among them, the expressions of TTF-1 protein and CC10 protein in dilated bronchiolar epithelium were significantly down-regulated, while that of P63 protein was up-regulated. Proliferation of progenitor cells under the epithelium mainly includes two modes, namely cubic epithelial hyperplasia (TTF-1 is mainly co-localized with SPC) and columnar epithelial hyperplasia (TTF-1 is mainly co-localized with P63 or CC10). The findings of this study reveal that aberrant proliferation and repair of airway progenitor cells are more common in the airways of patients with peripheral lesions. The above findings suggest that chronic airway inflammation and infection may promote aberrant proliferation of airway epithelial progenitor cells, which in turn promotes the development of a vicious circle. The clinical treatment of previous branch expansion is more focused on anti-infection and anti-inflammatory treatment, and few studies have focused on the aberrant proliferation and repair of airway epithelium. The findings of this study provide an important reference for the future search for therapeutic targets for bronchiectasis (reversing the aberrant proliferation of epithelial progenitor cells).