The team led by He Jianxing orally reports two key researches on early diagnosis of lung cancer at the ESMO conference
2022-09-161706
From September 9 to 13, 2022, as the most famous and influential oncology conference in Europe, the annual conference of the European Society for Medical Oncology (ESMO) was held as scheduled. At the conference, two researches conducted by the team led by professors He Jianxing and Liang Wenhua on early diagnosis of lung cancer was reported. The team was from the (National Center for Respiratory Medicine) of the First Affiliated Hospital of Guangzhou Medical University, the Guangzhou Institute of Respiratory Health and Laboratory. They respectively proposed a new screening mode for lung cancer and a highly accurate auxiliary diagnosis tool for pulmonary nodules, making the voice of China in the prevention and control of lung cancer heard by the world.
01 Proffered Paper Session: Community screening of lung cancer in Guangzhou
Background: Several studies have revealed that smokers can benefit from screening. However, lung cancer is commoner among women and non-smokers in Asia as compared with Europe and the US. Most current lung cancer screening studies are conducted on selected high-risk populations. Therefore, this study aims to evaluate the results of screening strategy in the general population of China, and find out the risk factors of lung cancer, so as to improve risk screening and estimation.
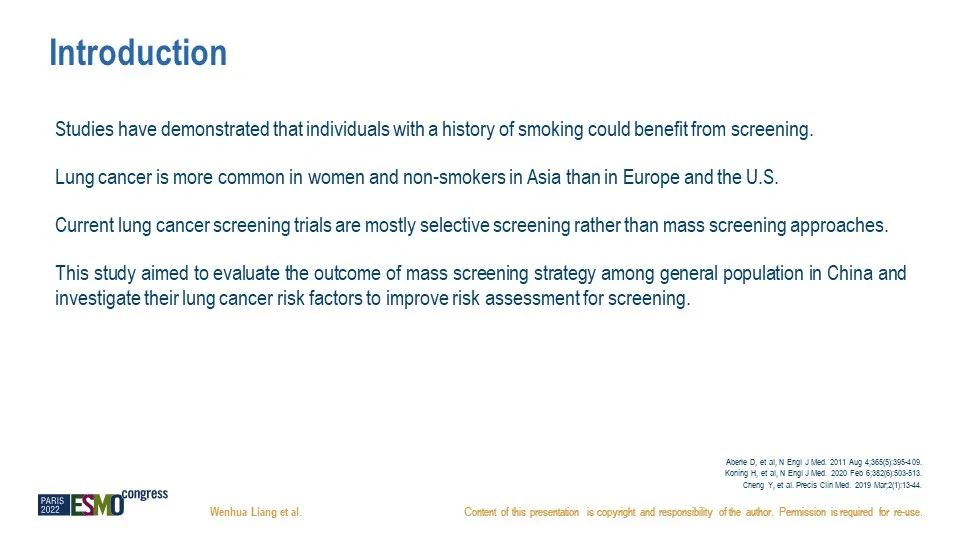

Result: From 2017 to 2021, residents ages between 40 and 74 without any medical history of lung cancer or lung cancer related symptoms from four communities in Guangzhou were recruited for LDCT lung cancer screening. A total of 11,708 residents received LDCT, and 230 residents received an invasive diagnostic procedure, including surgery. In the population receiving LDCT, 19.2% were discovered to carry significant solitary pulmonary nodules and 1.7% were identified with a pathologically proven lung cancer. 86% of lung cancer cases are in stage 0-1 where most cases are believed to be curable. The morbidity of lung cancer increases with age, peaking at ages 60 – 64. On the contrary, the proportion of stage I lung cancer decreases with age, suggesting that the balance between the lung cancer detection rate and the proportion of curable cases shall be considered in designing the screening.
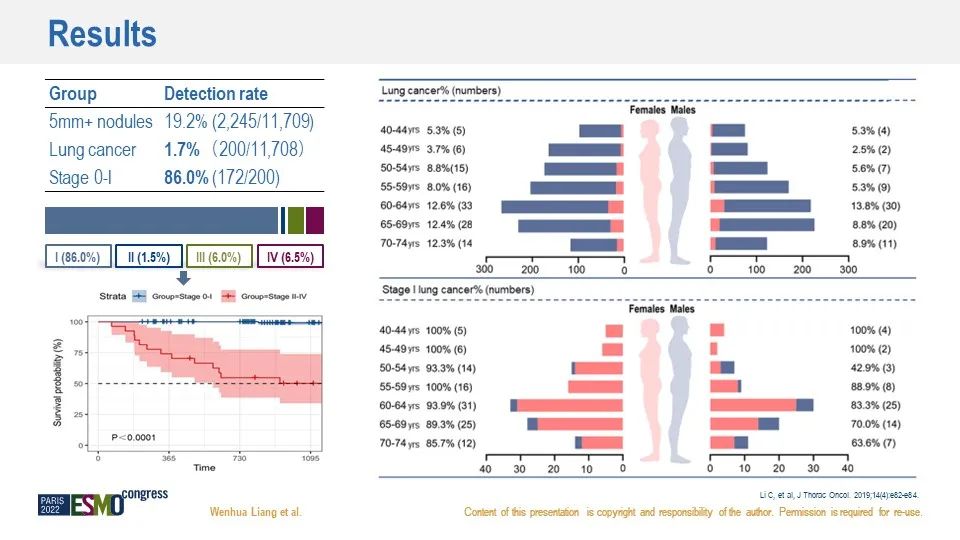
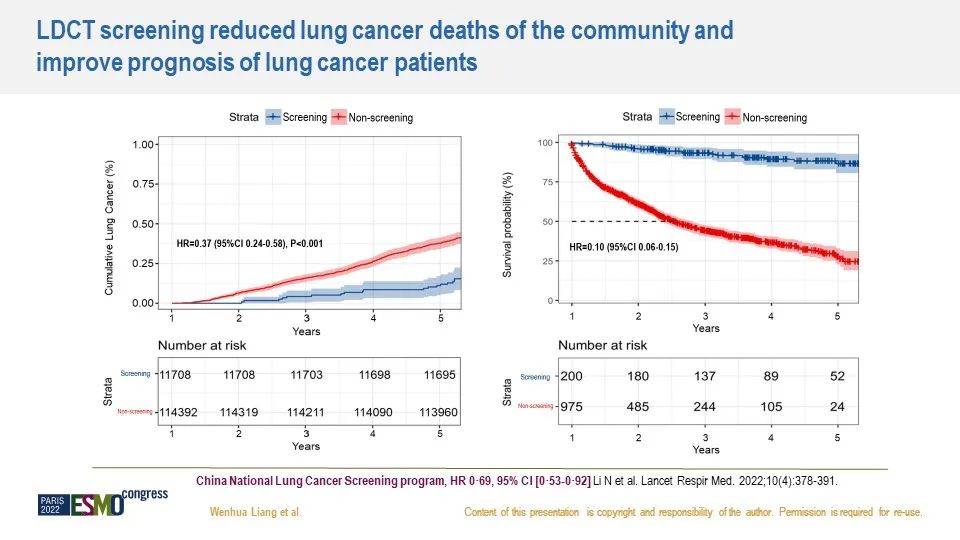
Using a non-screened population of approximately 110,000 residents from the same community as a control group, it was discovered that LDCT screening reduced lung cancer-related deaths by 63%, with a risk ratio (0.37) much lower than that of the national one-time screening project of China (0.69), which may be attributed to the inclusion of so-called non-high-risk populations. The lung cancer prognosis of the screened group was consistently better than that of the non-screened group, which may be attributed to a higher proportion of the cases in early stages.
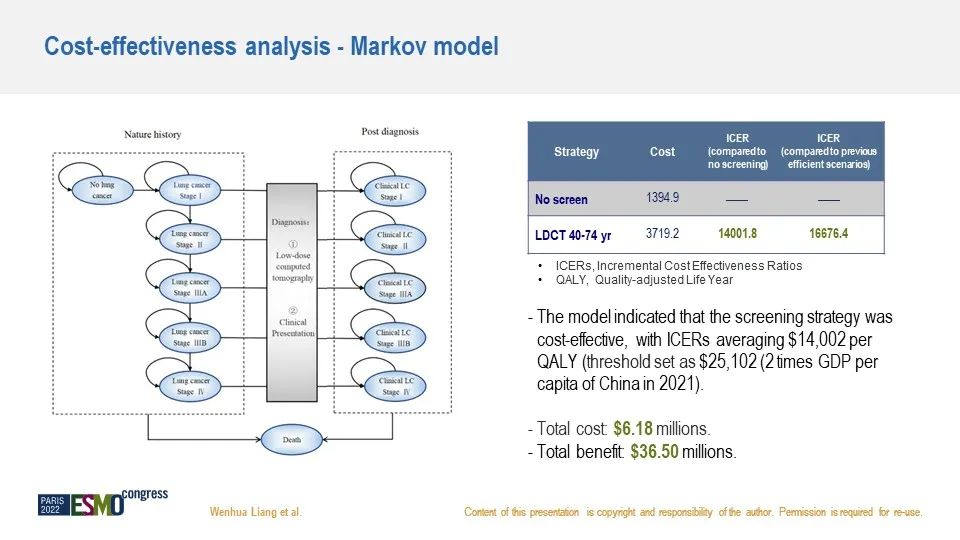
Using the Markov model, the general screening strategy is proven to be highly cost-effective, with an incremental cost-effectiveness ratio of $14,002 per quality-adjusted life year, less than twice the per-capita GDP of China. Furthermore, the cost of screening and subsequent treatment was estimated, and the total benefit was six times the cost compared with the non-screened group.
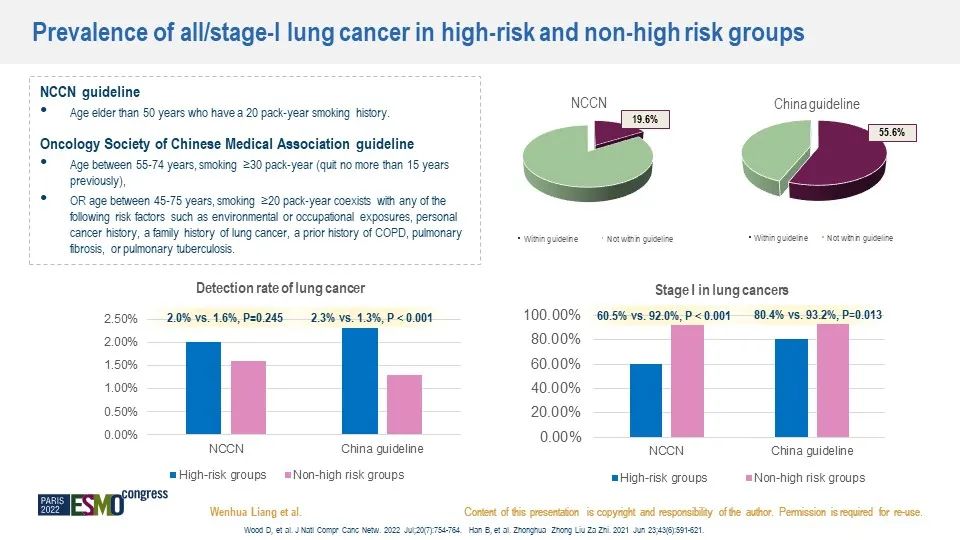
In patients diagnosed with lung cancer,Only 19.6% and 55.6% of patients detected with lung cancer met the criteria of NCCN guidelines and the Chinese consensus, suggesting that more than half of the detected lung cancer cases will have been missed if the restricted CT recipients meet the current criteria. There was no difference in detection rates between high-risk and non-high-risk populations as defined by the NCCN guidelines. The detection rate of the high-risk group is relatively high in China, but the detection rate of the non-high-risk group cannot be ignored. In addition, it was discovered that the proportion of lung cancer cases at Stage I was higher in the non-high-risk population according to these two criteria, suggesting that current criteria must be expanded to accommodate the lung cancer characteristics in China.
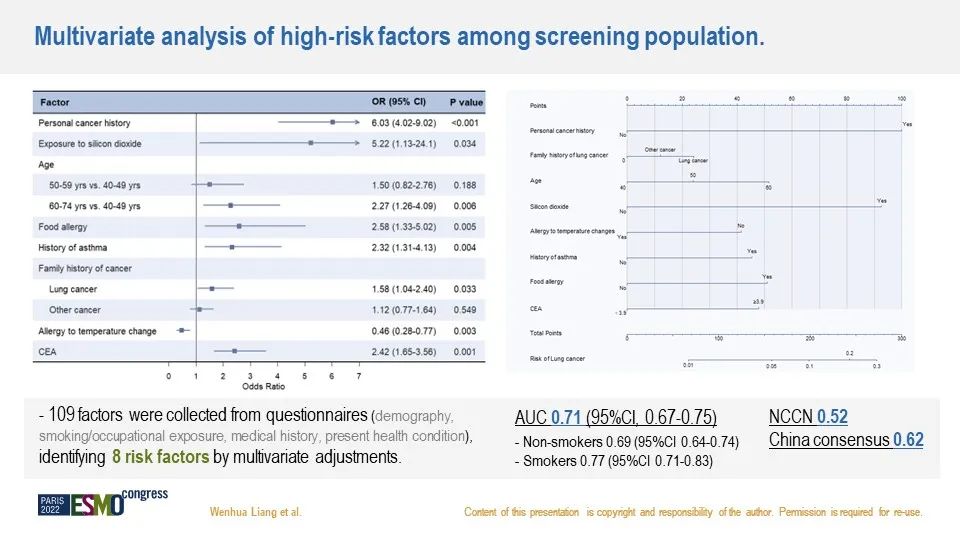
109 factors were collected from questionnaires involving demographics, smoking / occupational exposure, medical history, and current health status. After multivariate adjustment, the factors like personal history of cancer, silica exposure, old age, food allergy, asthma history, and family history of lung cancer were found to be independent risk factors, while hypersensitivity to temperature changes may be protective. With the aid of these significant variables and CEA (with a critical value of 3.9), the AUC of the comprehensive prediction model was 0.71, which was significantly higher than the criteria in the NCCN guidelines and the Chinese consensus.
Significance: In southern China, LDCT was proven to be able to identify early lung cancer and reduce lung cancer mortality. Considering the equal detection rate and the higher proportion of lung cancer cases under Stage I in the “non-high-risk” population compared with the high-risk population, the inclusion of the “non-high-risk” population is reasonable. By investigating and studying the risk factors, a risk prediction model was established to improve the risk assessment for lung cancer screening.
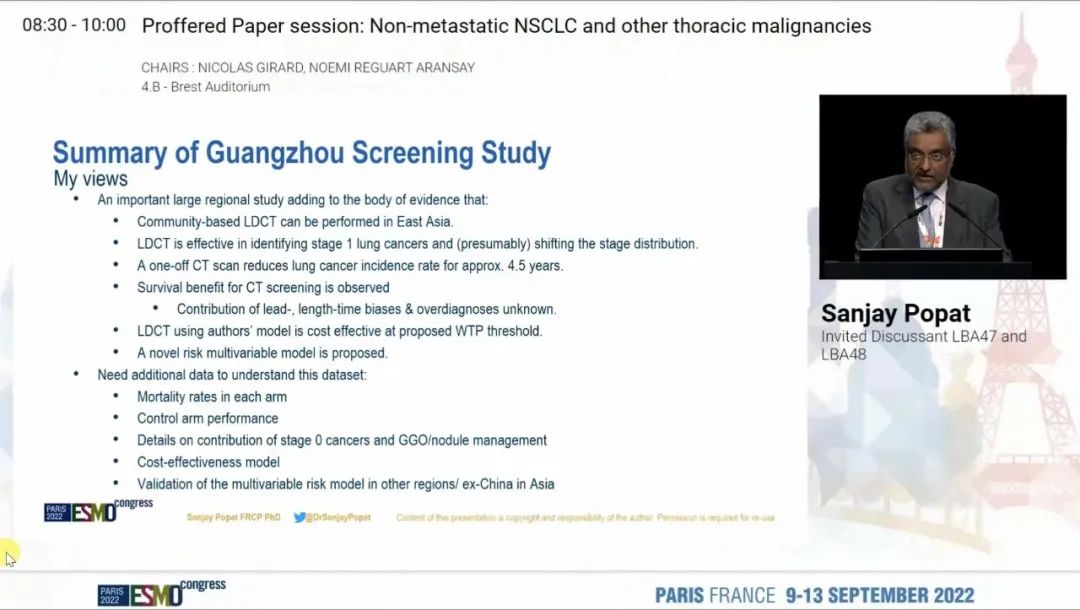
Expert comments: Professor Sanjay Popat, from Royal Marsden Hospital and Institute of Cancer Research, London, the UK commented that the findings were an important supplement to the current evidence system for lung cancer screening. The screening strategy can help detect more Stage I lung cancer cases.
02 Mini oral session: a combination of ctDNA methylation and image features for the diagnosis of lung cancer
Background: A lot of clinical needs for the accurate and noninvasive detection of the early diagnosis of lung cancer have not been met, and more and more pulmonary nodules have been diagnosed by CT. Previously, the research team has established and verified a blood-based DNA methylation model (PulmoSeek) through multiple centers to help address the problem. Theoretically, image features show better sensitivity to ctDNA non-fallen nidus, while ctDNA biomarkers are more specific. Thus, the two are complementary. Therefore, to further improve its diagnostic performance, the researchers have integrated ctDNA methylation, clinical features, and CT features to develop a combined model, PulmoSeek plus, for the classification of benign and malignant nodules. Meanwhile, a model based on 12 imaging features has been developed for invasiveness classification.
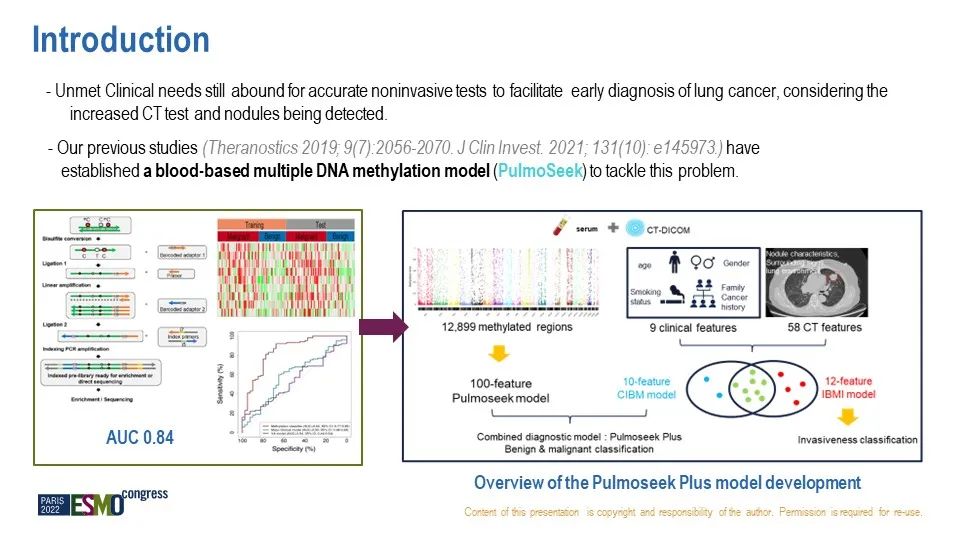
Result: About 1,300 patients with isolated pulmonary nodules were included through prospective specimen collection and retrospective blind assessment to develop a clinical and imaging biomarker model (named as CIBM) and ctDNA methylation model (called PulmoSeek).
The clinical and image CIBM model showed higher accuracy than the Mayo and Brock models in two independent cohorts, with an AUC of 0.85 and an overall accuracy of 80% in distinguishing AIS/MIA and IA. While the PulmoSeek Plus integrating ctDNA methylation and imaging CIBM models showed a better performance than the PulmoSeek and CIBM models alone, with AUC improved by 6% and sensitivity improved by 5-6%. PulmoSeek Plus was sensitive to 98% of nodules of different sizes and was superior to PulmoSeek used alone.
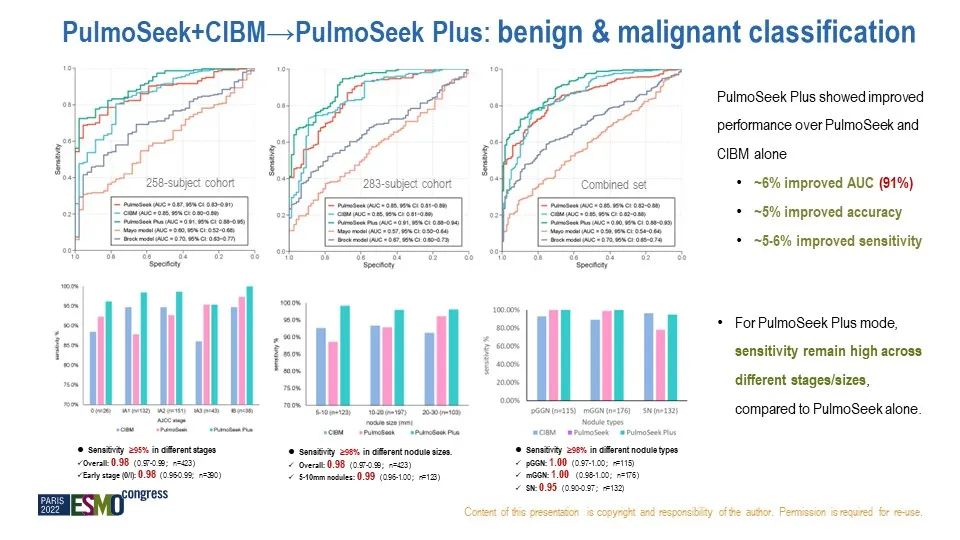
Decision curves showed that the PulmoSeek Plus model had the best net clinical benefit among the five existing models. In the clinical application of PulmoSeek Plus, the low cutoff values with high sensitivity and high cutoff values with high specificity were both applied to divide the uncertain lung nodules into low, medium and high risk groups. Through reclassification, PulmoSeek Plus can reduce unnecessary surgery by 89% and delayed treatment by 73%.
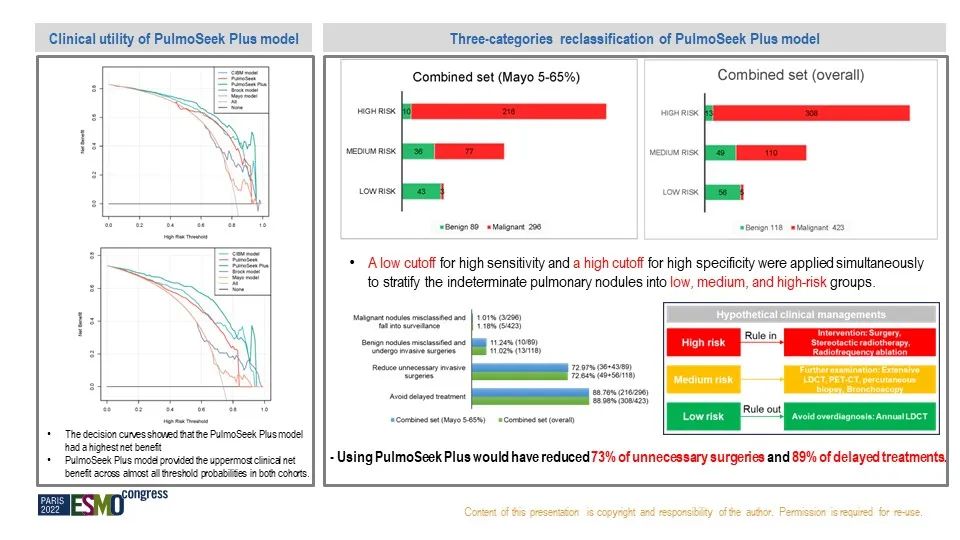
PulmoSeek Plus is a model integrating clinical, imaging, and DNA methylation biomarkers. With high precision and high sensitivity, the model is superior to any model based on any single factor. PulmoSeek Plus may be the best tool available for the diagnosis of pulmonary nodules.
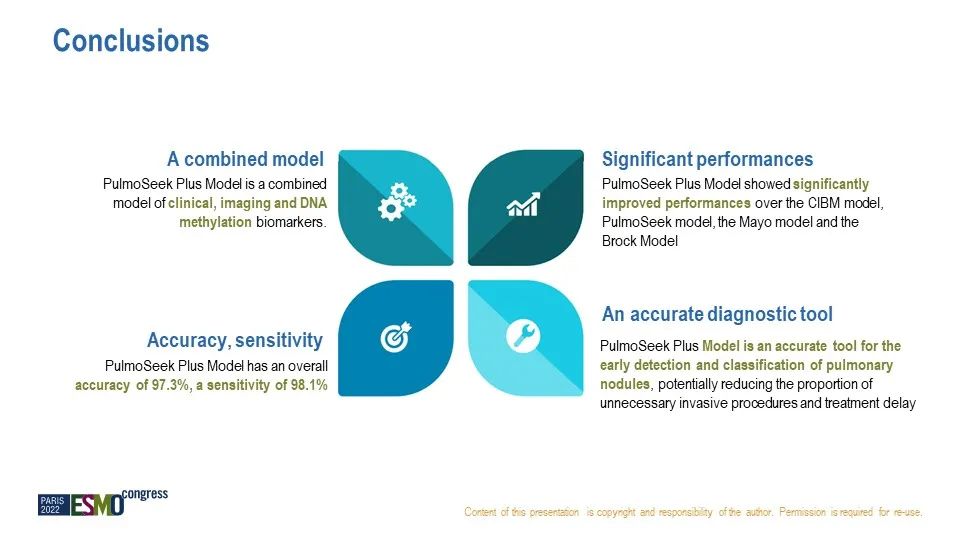
Significance: It has confirmed that clinical imaging features and ctDNA methylation and other forms of markers can complement each other. Through the new model integrating clinical, imaging and DNA methylation biomarkers, it can be used to improve the differential diagnosis of pulmonary nodules, so as to minimize the overtreatment and treatment delay of the growing population of patients.
Expert comment: Professor Sarah-Jane Dawson, from Peter MacCallum Cancer Center, Melbourne, Australia, suggested that ctDNA methylation can be used to diagnose cancer efficiently, and that the integration of markers at different levels is of great significance for the early diagnosis of lung cancer.
03 A new screening mode for lung cancer and a new means of early diagnosis
The above two associated studies are of great significance to lung cancer prevention and control in China and worldwide:
According to the pathogenic characteristics of lung cancer in Chinese population, the inclusion of “non-high-risk” population into the screening has for the first time shown the value of general screening strategy to Chinese population, which may be more reasonable than high-risk screening strategy, and help discover more lung cancer cases under the curable stage, suggesting that the screening criteria for Chinese people should be further improved.
Considering the “side effect” of the high false-positive rate of CT screening, a combined lung cancer diagnostic model integrating ctDNA methylation and imaging characteristics was developed for the first time, which proved the complementarity of markers at different levels and improved the accuracy to more than 90%, effectively reducing the excessive and delayed diagnosis and treatment of “uncertain” pulmonary nodules.