Special Talk of CHEST Journal: An Interview with Professors Guan Weijie and Wang Deyun
2023-05-221404
The latest issue of Chest Journal Podcast had an interview with Research Fellow and Principal Investigator Guan Weijie with the State Key Laboratory of Respiratory Disease and Professor Wang De Yun with the University of Singapore on the article Motile Ciliary Disorders of the Nasal Epithelium in Adults with Bronchiectasis published in May (for the previous report of the article, please refer to the Nanshan Respiration Website “Research progress of bronchiectasis (I): the discovery of common existence of abnormal expression of ciliary markers in upper airway, published by Chest”, with the link of https://mp.weixin.qq.com/s/yuf8Y3I2h5JoM0P3vygn1g). Chest Journal Podcast is an interview program for the journal CHEST to discuss with the authors of articles from the current issue, adding context and commentary to the challenges facing clinicians in the fields of pulmonary, critical care, and sleep medicine.
Dr. Gretchen Winter with the American Society of Chest Physicians, as the editor of the Podcast column, had an in-depth discussion on the research design, content and significance of the mentioned article.
Here is an excerpt from the interview:
Q1: What is the significance of your research?
A1: Ciliated cells are the most important component of the first defense barrier of the airway. Previous studies have found that motile ciliary disorder not only occurs in primary ciliary dyskinesia (PCD), but also is manifested in many other chronic airway inflammatory diseases (such as asthma and allergic rhinitis). According to the vicious vortex hypothesis, the airway mucociliary clearance dysfunction will damage the host’s normal defense function and increase the susceptibility of the respiratory tract to pathogens (Figure 1), which will cause inflammatory response, lead to airway damage and remodeling, and promote the occurrence and progression of bronchiectasis. Therefore, motile ciliary dysfunction may be a common clinical phenomenon and associated with the severity of bronchiectasis. This study aims to find out the association between airway defense function defects and bronchiectasis, explore the possibility of motile ciliary disorders as a means of diagnosis, and explore new targets for therapy.
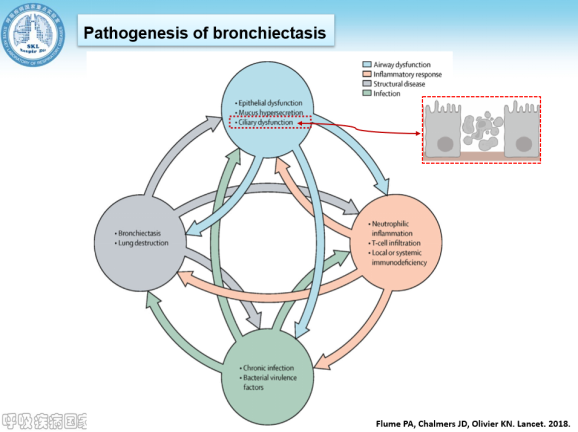
Figure 1. The vicious vortex hypothesis of bronchiectasis
Q2: What have you discovered about the relationship between motile ciliary disorder and bronchiectasis?
A2: Our study has found for the first time that the proportion of bronchiectasis patients with motile ciliary disorder was higher than expected (> 85% of bronchiectasis patients have immunofluorescent staining abnormality for at least one cilia marker, Figure 2). The research team initially intended to find out the preliminary evidence of the existence of motile ciliary disorder in bronchiectasis, but the results showed that motile ciliary disorder was a common phenomenon in bronchiectasis.
Figure 2. MCD is common in bronchiectasis
Q3: How do you determine that your findings connected with secondary MCD different from PCD?
A3: Most clinicians believe that ciliary dysfunction is congenital (related with genetic mutation) rather than secondary dysfunction. However, the latest results of our study demonstrate that most ciliary dysfunctions are secondary (accounting for 2 / 3 of the study subgroup, Figure 3). This suggests that ciliary dysfunctions may be more commonly caused by the damage due to chronic bacterial or viral infections or inflammatory mediators. Therefore, primary ciliary dysfunction is only one of the causes of the ciliary dysfunction.
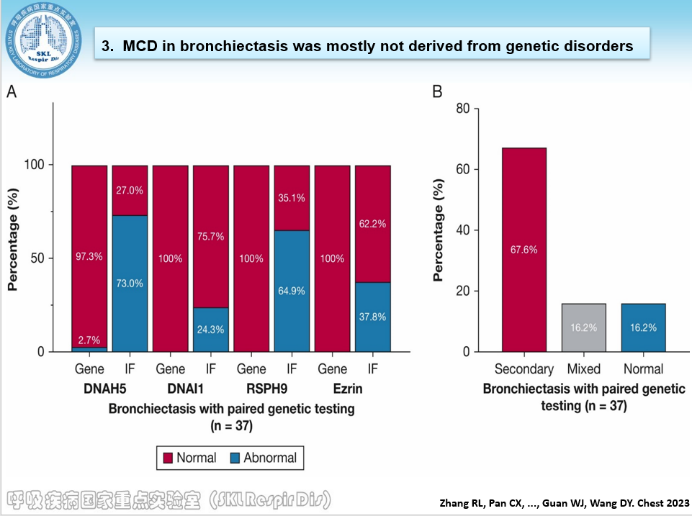
Figure 3. Ciliary dysfunction is mostly secondary lesion
Q4: What's the significance of these research findings? How do you apply your findings to clinical practice? Do you believe this will facilitate diagnosis or treatment of bronchiectasis?
A4: As mentioned above, clinicians have long mistakenly assumed that most motile ciliary disorders stem from primary ciliary dysfunction (PCD). Although immunofluorescence assay cannot easily distinguish between primary and secondary ciliary dysfunction, clinicians can be provided with the probability or extent of motile ciliary disorder. According to the theory of “the same airway with the same disease”, the MCD in the upper respiratory tract can actually effectively reflect the MCD in the lower respiratory tract to a certain extent. Therefore, we believe that nasal swab exam will have great potential for application in clinical diagnosis.
Q5: Can you talk about the limitations of this study?
A5: This study still has the following limitations: 1) the sample size of matched specimens from upper and lower airways is small, and the ciliary markers selected for the study is also limited; 2) immunofluorescence assay cannot directly reflect the cilia beating ability, but it can be regarded as an important alternative. 3) Due to the limited number of sample cells collected by nasal swab, further qPCR verification cannot be performed temporarily.
Q6: What do you think is the unique contribution of this study?
A6: As mentioned above, ciliary dysfunction is quite common in patients with bronchiectasis, most of which are secondary changes. This should be the most unexpected of all findings. Our study has also found that the most results of fluorescent assays on cilia were highly reproducible over time and largely consistent between upper and lower airways, which suggested the independence of the comorbidity of upper and lower airways or airway inflammation. These findings provide strong evidence that “the characteristics of upper airway can reflect the diseases at the lower airway”. Furthermore, this study has found that ciliary dysfunction is only weakly associated with the severity of bronchiectasis. Although the exact mechanism remains unclear, this is most likely because ciliary dysfunction has existed in patients when mild bronchiectasis (a significant proportion of patients with mild bronchiectasis show a significant eosinophilic inflammatory response in airway).
In addition, the above research findings were reported and shared by Dr. Pan Cuixia (supervisor: Prof. Guan Weijie) at the third European Bronchiectasis Workshop held in February this year, and Dr. Amelia Shoemark, an expert in ciliopathy research, asked questions and started discussions on the report.