Progress in Bronchiectasis Research: Advances in pharmacotherapy for bronchiectasis in adults
2023-05-292150Invited by Professor Rayya Hajjar, chief editor of the journal Expert Opinion On Pharmacotherapy (IF: 4.1), the research team of bronchiectasis published a special review entitled “Advances in pharmacotherapy for bronchiectasis in adults” in May 2023, instructed by the Research Fellow Guan Weijie.

Bronchiectasis is a chronic airway inflammatory disease with structural damage caused by the impaired airway defense function, with a pathological characteristic of irreversible bronchial dilation. The clinical manifestations include chronic cough, large sputum expectoration, intermittent hemoptysis, with or without shortness of breath, etc.. It is a heterogeneous disease that incurs huge social and economic burdens. The vicious vortex hypothesis is believed to be the pathophysiological pathogenesis of bronchiectasis, composed of impaired airway defense, chronic infection, chronic inflammation, and airway damage. Therapy in hospitalization for bronchiectasis patients mainly includes antibiotics, mucoactive medications, and bronchodilators with the aim of controlling airway infections, enhancing mucociliary clearance and lung function. Exploring new therapeutic targets can facilitate the individualized treatment of the patients to restrain the progression of the disease.
In this review, the authors retrieved and reviewed the studies on pharmacotherapy of bronchiectasis in MEDLINE, Web of Science, and ClinicalTrials.gov registry, summarized and evaluated such aspects as antimicrobial treatment, mucoactive medications and bronchodilators, anti-inflammatory treatment and treatment for etiology, and pointed out that the personalized treatment targeted phenotypes and underlying pathogenesis was an important direction of clinical treatment for bronchiectasis in the future.
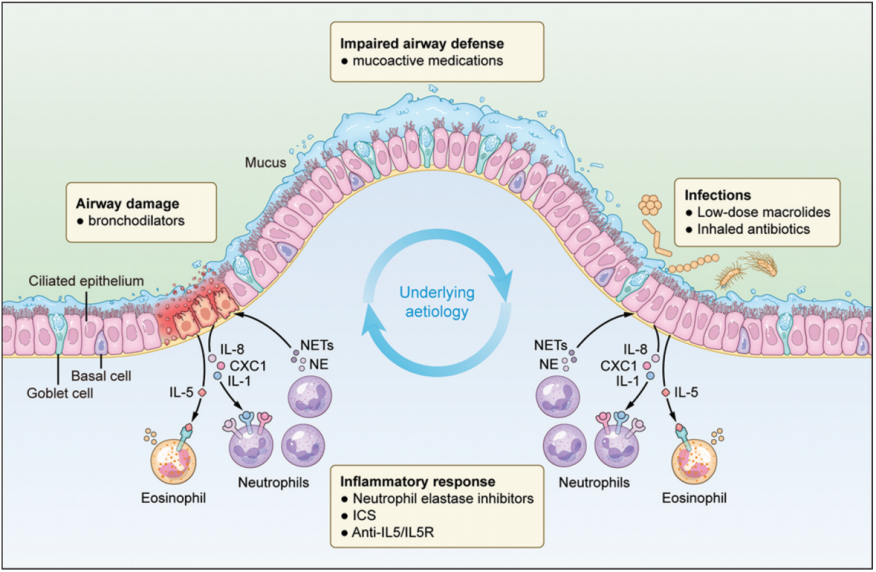
Figure 1: The pathogenesis of bronchiectasis and potential targets for drug therapy according to the vicious vortex hypothesis
Note: The vicious vortex hypothesis assumes the interaction of four cardinal interdependent components - impaired airway defense, chronic infection, chronic inflammation, airway damage, and the initial trigger of the cycle (the underlying etiology).
ICS: inhaled corticosteroids; NETs: neutrophil extracellular traps; NE: neutrophil elastase; IL: interleukin; IL5R: interleukin 5 receptor.
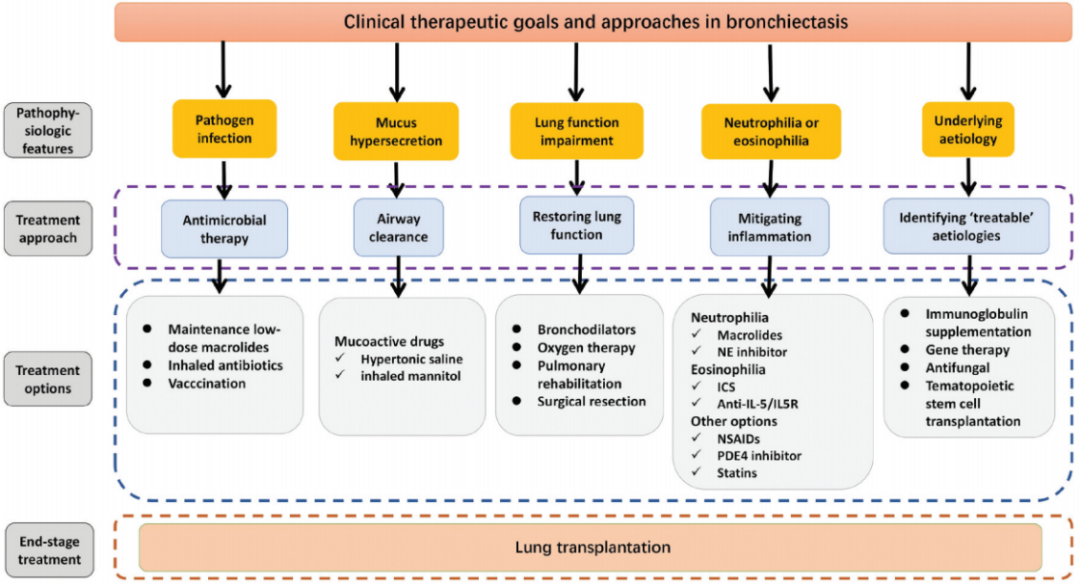
Figure 2: Treatment strategies for bronchiectasis
Note: √, Recommended by clinical trials.
Antimicrobial treatment
Airway bacterial infection is the core element of the vicious vortex hypothesis of bronchiectasis. Short-term, intermittent and even long-term antibiotics treatment may help block the vicious vortex. Macrolides have antibacterial, anti-inflammatory and immunomodulatory effects. Long-term low-dose use of macrolides can help reduce the risk of acute exacerbation of bronchiectasis and improve lung function and quality of life to varying extent. Inhaled antibiotics have the advantages of low drug resistance and a high drug deposition rate in the lungs. In adults with bronchiectasis, inhaled antibiotics has been conditionally recommended by the 2017 European Respiratory Society guidelines for patients with bronchiectasis – patients with at least three exacerbations per year and chronic lung infections with P. aeruginosa are deemed the candidates with optimal therapeutic outcomes. A phase III national randomized controlled trial demonstrated that tobramycin aerosol inhalation significantly reduced the load of Pseudomonas aeruginosa in sputum and improved the quality of life of patients.
Mucoactive medications and bronchodilators
Clinically, mucoactive medications can be prescribed on the basis of chest physiotherapy, mainly including inhaled mannitol, recombinant human deoxyribonuclease donnase (rhDNase), inhaled hypertonic saline and normal saline, chloride ion channel potentiators, etc., which can improve the physical properties of sputum and the cough clearance, reduce the risk of bacterial colonization in sputum, improve lung function and quality of life. Furthermore, bronchodilators can significantly improve the lung function of dyspnea patients.
Anti-inflammatory therapy and etiological therapy
Defining the inflammatory endotype of bronchiectasis patients is the key to implementing precise anti-inflammatory therapy, and individualized anti-neutrophil therapy is an important direction of future treatment. A phase II randomized, double-blind, placebo-controlled trial demonstrated that oral administration of dipeptidyl peptidase-1 (DPP-1) inhibitors significantly reduced the neutrophil level in sputum and significantly postponed the first exacerbation. In patients with type II airway inflammation with significantly elevated eosinophil counts, glucocorticoids reduced the sputum production, while anti-IL-5 or anti-IL-5 receptor monoclonal antibody therapy reduced the frequency of acute exacerbation and improved the lung function and quality of life. Gene therapy is an important direction for the treatment of primary ciliary dyskinesia. In patients with allergic bronchopulmonary aspergillosis, the administration of corticosteroids, antifungal agents, or biological agents can effectively improve the clinical outcome.
Summary
Currently, there is still a lack of effective therapeutic strategies for the vicious vortex of bronchiectasis. More researches and trials are needed to reveal the underlying mechanisms, and the animal models of bronchiectasis will facilitate the development of new drugs. In conclusion, the pharmacotherapy for bronchiectasis has made significant progress in the last decade, but there are still many challenges. Personalized therapy targeting the phenotypes and specific pathophysiology is an important direction for future treatment.
Research Fellow Guan Weijie is the corresponding author of the review, and Dr. Zhang Xiaoxian, Dr. Chen Zhaoming, and Dr. He Zhenfeng are the co-first authors. This research is supported by the National Natural Science Foundation of China Outstanding Youth Foundation, the General Program of National Natural Science Foundation of China, the General Program of Guangdong Natural Science Foundation, Nanshan Medical Foundation, Guangzhou Science and Technology Plan Project, and the National Outstanding Youth Foundation of Guangzhou Medical University.
References
Zhang XX, Chen ZM, He ZF, Guan WJ. Advances in pharmacotherapy for bronchiectasis in adults. Expert Opin Pharmacother. 2023 May 9:1-15. doi: 10.1080/14656566.2023.2210763. Epub ahead of print. PMID: 37161410.