The Research Team Led by Professor Yang Zifeng Reveals the Coinfection of Influenza Virus and Bacteria Aggregates Inflammatory Lung Injury and Alters Gut Microbiota in COPD Mice
2023-03-231607The research team led by Professor Yang Zifeng with the SKLRD, the team led by Professor Yang Weimin with Kunming Medical University, and the team led by Professor Xia Xueshan with Kunming University of Science and Technology jointly studied the pathogenic mechanism behind the acute exacerbation of COPD mice caused by cigarette smoke exposure and coinfection with influenza virus and non-typeable Haemophilus influenzae (NTHi), and found that infection aggregated the inflammatory lung injury, and altered the gut microbiota in COPD mice. The paper “Coinfection with influenza virus and non-typeable Haemophilus influenzae aggregates inflammatory lung injury and alters gut microbiota in COPD mice” was accepted by the journal Frontiers in Microbiology on March 16, 2023.
Acute exacerbation is closely associated with COPD mortality. Among them, infection is the main cause of acute exacerbation of COPD (AECOPD), as about 70~85% of AECOPD cases are related with respiratory viral and bacterial infections, and the co-infection cases of the two account for 6.5~27% of AECOPD. Studies have revealed a synergistic relationship between influenza viruses and bacteria, and that influenza can increase the susceptibility and severity of secondary bacterial infections. Moreover, increasing evidences suggest an association between the gut and respiratory tract, and the interaction between gut microbiota and host immunity can influence the disease progression. However, it is still unknown how coinfection in AECODP affects the host’s inflammatory response and gut microbiota composition.
In this study, a COPD mice model was constructed using a mouth-nose cigarette smoke exposure system to further induce acute exacerbation in mice with H1N1 influenza virus and NTHi. The results showed that coinfection with H1N1 and NTHi caused a higher mortality, more severe inflammatory infiltration in the lung, and a more significant decline in lung function in COPD mice. H1N1 enhanced the proliferation of NTHi, while NTHi had no effect on H1N1 replication. Furthermore, co-infection promoted the recruitment of macrophages, M1 type macrophages, neutrophils, monocytes, NK cells, and CD4 + T cells to the lungs, and caused the depletion of alveolar macrophages. Co-infection also caused reduced diversity of gut microbiota in COPD mice, where Muribaculaceae, Lactobacillus, Akkermansia, Lachnospiraceae and Rikenella genera showed a negative correlation with lung cytokines, while Bacteroides showed a positive correlation with cytokines.
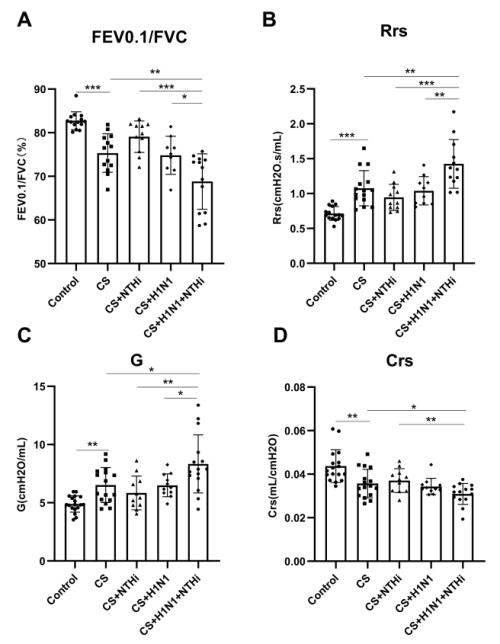
Figure 1. Coinfection exacerbated the decline in lung function of COPD mice
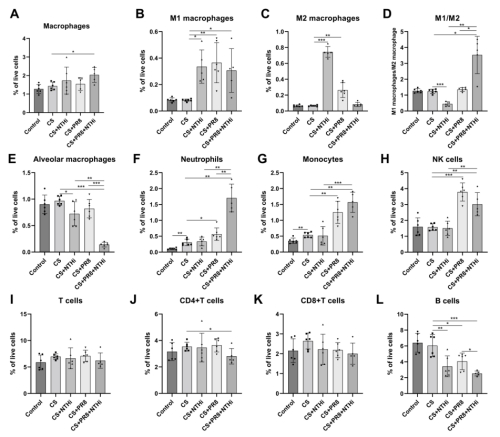
Figure 2. Coinfection affecting the immune cells in the lungs of COPD mice
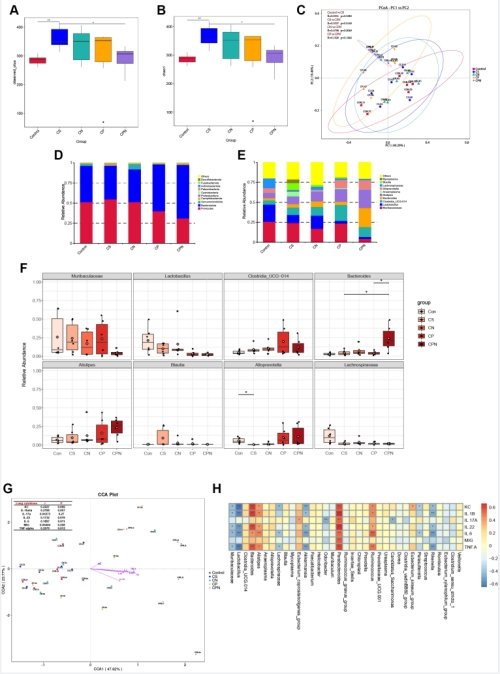
Figure 3. Coinfection-induced dysregulation of gut microbiota in COPD mice was associated with cytokine expression in the lungs
Professor Yang Zifeng, Professor Yang Weimin from Kunming Medical University and Professor Xia Xueshan from Kunming University of Science and Technology are the joint corresponding authors of this paper. Doctoral candidate Wu Xiao, Dr. Li Runfeng and Professor Lin Zhengshi are the co-first authors of this paper. The project was supported by projects such as National TCM Multi-disciplinary Innovation Team Project and the National Natural Science Foundation of China.