A Review on Cough in Asthma Published by Professor Lai Kefang with Other International Experts
2023-06-295127
Characteristics and phenotypes of cough in asthma
Two thirds of adult patients with cough-variant asthma (CVA) are dry cough cases. Child patients with wet cough are likely to be misdiagnosed as asthma. Nocturnal cough is a prominent feature of asthma in adult patients, which can be detected in more than 50% of adult patients with asthma. Only a third of child patients with nocturnal cough are diagnosed as asthma.
Based on cough symptoms, asthma can be classified into CVA, cough-predominant asthma (CPA) and typical asthma or wheezing-predominant asthma (WPA). CVA’s only symptom is chronic cough, without any typical asthma symptoms such as wheezing or dyspnea, which accounts for up to 33% of the causes of chronic cough. Although CPA patients have the symptom of wheezing, wheezing is a mild or transient symptom, while cough is their persistent and significant symptom. Patients with WPA mainly show symptoms of wheezing or dyspnea, with little or no cough. Due to the similarities between CVA and CPA in pathogenesis, clinical manifestations and treatment, the authors propose that CVA and CPA are collectively referred to as asthmatic cough or cough associated with asthma.
Assessment of cough in asthma
Currently, the parameters of the scale assessing the severity of acute asthma in children do not cover cough. Among the assessment tools for children’s asthma control and asthma-specific quality of life, only one of the seven questions in Asthma Control Test (ACT) was related to cough, and the cough score contributed little to the total score. In the five-question version of ACT, there were no cough-related questions. The adult asthma control assessment tools (e. g. ACQ or ACT) do not contain any cough-related questions. There is a question about cough in the Asthma Quality of Life Questionnaire (AQLQ), but the relevancy of individual score has not been verified.
In children and adults with cough and asthma, the first step is to objectively ascertain the diagnosis of asthma by either reversible airflow obstruction or airway hyper-responsiveness (BHR). After the diagnosis of asthma, the assessment should focus on:
(1) Core treatable trait assessment (type 2 inflammation and airflow obstruction)
(2) Differential diagnosis or identification of clinical conditions causing or affecting cough;
(3) Assessment of cough
Evaluation of asthmatic cough in children includes its duration, character (wet or dry, metallic or paroxysmal), etc. Objective asthma markers include spirometry, presence of airway hyper-responsiveness, and fractional exhaled nitric oxide (FeNO).
Evaluation of asthmatic cough in adults requires identification of treatable features associated with cough, such as type 2 inflammation, airflow obstruction, etc. Medical history collection should cover cough duration, temporal pattern, cough triggers, and associated symptoms. Nocturnal wheezing and worsened cough supported the diagnosis of asthma. Cough reflex sensitivity can be assessed by tussigenic inhalation challenge tests, cough severity can be assessed with 0-100 Visual Analogue Scale (VAS) score, and the effect of cough on quality of life can be assessed with the Leicester Cough Questionnaire (LCQ). Increased cough frequency and worse FEV1 are independent predictors of asthma control, indicating that cough frequency and airflow obstruction represent independent dimensions of asthma control, and technological advances in objective cough monitoring will further promote researches on cough assessment and management.
The pathophysiology and mechanisms of phenotypes of cough in asthma
Previous studies have found cough hypersensitivity in adult patients with stable asthma, and increased capsaicin cough response was associated with more severe asthma in patients with non-atopic asthma, which is possibly due to altered sensory nerve excitability and activity of the upper-airway laryngeal vagal sensory nerve fibres driven by the inflammatory pathology of asthma. vagal and trigeminal inputs converge on the nucleus of the solitary tract, leads to altered synaptic efficacy in the brainstem, which is part of a process of central sensitisation that includes increased activity in the midbrain areas in chronic cough, with a reduced ability to supress coughing(Figure 1). However, these mechanisms remain to be established.
Cough is usually the commonest complaint of asthma during respiratory infections. Cough induced by external physical and chemical factors is associated with an increased risk of asthma. Epithelial damage, mucus hypersecretion, release of inflammatory cytokines, deficiency in interferon-γ, and interleukin (IL)-12 might be the basis for the hypersensitisation and hyper-responsiveness of airway nerve fibres
Smooth muscle constriction induced by asthma mediators, such as histamine and cysteinyl leukotrienes may be an important mechanism of asthmatic cough. It is speculated that due to the effect of acute bronchoconstriction in releasing mediators, such as ATP, that sensitise capsaicin-responsive cough airway nerves. Mechano-sensitive afferent airway nerves might be activated by bronchoconstriction and interact with those evoking cough in the brainstem.
When a lung allergen challenge was used in steroid-naive adults with atopic asthma, the capsaicin-evoked cough sensitivity has increased and was found to be associated with the increase of sputum eosinophilia, which can interact with airway nerves. Among the moderate to severe asthma patients with higher degree of eosinophils, There was a greater colocalisation of substance P, eosinophils, and airway nerves in bronchial biopsies. Cough and capsaicin cough sensitivity can be improved with anti-IL-5 antibody in patients with severe eosinophilic asthma, suggesting that eosinophilic inflammation may underlie the chronic cough and cough hypersensitivity of corticosteroid-resistant cough in asthma.
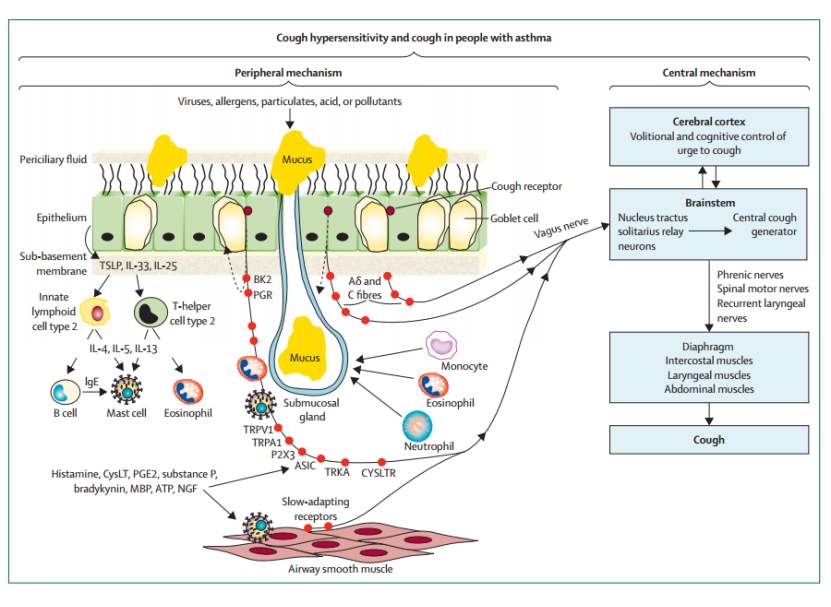
Figure 1: Peripheral and central mechanisms underlying cough hypersensitivity and cough in people with asthma
Peripheral mechanism: innervation at the surface epithelium of the larynx, trachea, and main bronchi, including mucous glands and airway smooth muscle, with sensory neurons mediating cough. Vagal Aδ fibres are activated by mechanical stimuli (eg, inhaled particulate matter, mucus, and protons); vagal C fibres are activated by irritant chemicals and inflammatory mediators released from eosinophils, mast cells, and epithelial cells. Vagal fibres contain several ion channels and receptors. In addition, these mediators can cause bronchoconstriction, which can activate cough vagal fibres through activation of slow-adapting receptors. Eosinophils and mast cells might interact directly with vagal cough fibres to increase nerve fibre density or by releasing neuroactive mediators directly to nerve fibres. Type 2 inflammation, typical of asthma, results from the release of alarmins from epithelial cells (TSLP, IL-33, and IL-25) that activate innate lymphoid cell type 2 and T-helper cell type 2 to release IL-4, IL-5, and IL-13, which induces eosinophilic inflammation and activation of B cells to produce IgE and sensitise mast cells.
Central mechanism: vagal fibres project to brainstem nuclei to coordinate motor patterning for cough. In the higher cortical and subcortical areas of the brain, networks are involved in the behavioural regulation of cough, encoding of the urge to cough, and processing of cognitive and affective responses. These networks allow volitional and cognitive modulation of cough through top-down regulation of brainstem processing, and these central pathways might be sensitised, contributing to cough hypersensitivity. ASIC=acid-sensing ion channel. BK2=bradykinin type 2 receptor. CysLT=cysteinyl leukotriene. CYSLTR=cysteinyl leukotriene receptor. IL=interleukin. MBP=major basic protein. NGF=nerve growth factor. P2X3=P2X purinoceptor 3. PGE2=prostaglandin E2. PGR=prostaglandin receptor. TRKA=tyrosine receptor kinase A. TRPA1=transient receptor potential ankyrin 1. TRPV1=transient receptor potential cation channel subfamily V member 1. TSLP=thymic stromal lymphopoietin.
Management of cough in adults with asthma
Asthmatic cough in adults is heterogeneous, involving multiple different pathophysiological mechanisms. We should follow the treatable trait treatment model to achieve individualized treatment:
(1) For asthmatic cough patients with bronchoconstriction and type 2 inflammation, inhaled corticosteroids and long-acting β-adrenoceptor agonists are effective in relieving cough, and single inhaler maintenance and reliever therapy (SMART) may be equally effective for cough in asthma because of its effects on both airway smooth muscle and type 2 inflammation. For patients using inhalation therapy, it should be assessed whether they have mastered the correct inhalation method.
(2) For cough patients with cough hypersensitivity, to identify and manage cough triggers and comorbid diseases associated with persistent cough and, second, to control cough hypersensitivity. LAMA treatment is effective to some patients with tolerance to ICS / LABA treatment. The use of anti-IL-5 antibody mepolizumab for severe eosinophilic asthma can improve cough symptom and hypersensitivity. Speech pathology and physiotherapy techniques, hydration, inhaled tiotropium, and inhaled menthol, and neuromodulators such as gabapentin can be considered. A P2X3 receptor antagonist (gefapixant) may be effective in the treatment of chronic refractory cough.
(3) Patients with asthmatic cough with mucus hypersecretion can be treated with airway clearance techniques and low dose azithromycin.
(4) When cough in asthma is still not relieved through specific treatment, the cough should be re-evaluated to confirm whether there are important comorbid diseases related to asthma, such as rhinosinusitis, laryngeal dysfunction, bronchiectasis, gastroesophageal reflux disease, obstructive sleep apnea syndrome, large airway collapse or excessive dynamic airway collapse, etc.
Management of cough in children with asthma
For child cough patients (<18 years old) diagnosed with asthma, environmental exposure factors should be assessed first. If the cough is acute (with a duration <2 weeks) or subacute (with a duration of 2-4 weeks), with other symptoms and signs like an acute attack and poor control of asthma, the acute asthma should be managed according to local guidelines; if there are no asthma related symptoms and signs, or the cough still cannot be relieved after 2-4 weeks of comprehensive management, the presence of other causes of acute cough should be considered. For chronic cough (duration> 4 weeks), assessment and management according to the guide to pediatric chronic cough can be conducted or examinations like FeNO, pulmonary function, and induced sputum can be performed; if no asthma markers are found, observation, reassessment or experimental anti-asthma therapy can be adopted after consulting with the patients’ family. In addition, due to the lack of evidence of efficacy and substantial adverse events, cough relieving drugs such as opiates, amitriptyline, gabapentin are not recommended for child patients.
Prospect
All the time, cough in asthma has long been neglected as a symptom that could be a measure of asthma control. Therefore, we know very little about the extent of cough, the pathogenesis, and how to treat it in asthma patients. However, in the last decade, the concept of cough hypersensitivity has been put forward, and progress has been observed in researches such as the neurogenic inflammatory process leading to peripheral and central sensitization. In such a context, cough and cough hypersensitivity should be considered as a treatabletrait of asthma.
For a better treatment of cough in asthma, our future researches should focus on discovering the patterns of cough in asthma, re-assessing cough as a symptom of asthma control, establishing the effects of current asthma treatments including, and understanding the mechanisms of cough in asthma.